March 2024 blog
Tories: (and Labour) You've been lying when you oughter be truthin'
Thatcher planned end of NHS a detailed article from released archives
Thatcher brought in purchaser/provider
so any profiteering cowboy outfit could take public tax funds to make profits...
Milburn brought in "Any (Un)Qualified Provider"
The Tory government have slipped through
the introduction of Physician Associates and Anaesthetic Associates (neither
physicians, nor Anaethetists)
in a side committee with a Tory majority, and MPs have voted it through on the
nod…
The GMC have been coerced into registering PAs, AAs, but so far will not regulate them.
Trusts will not enforce safe supervision-and a two tier NHS has been formed...
The ARRS contract makes it impossible for a GP practice to hire new GPs, but reimburses for PAs
Several GP practices have sacked GPs,
employing PAs
and several GP practices have closed.
Thus the Torys have demoted GP practices
by underfunding, introducing non-doctor staff-some saying “if you will
not accept a PA, we cannot see you”
Just like Centene practices-supervision remotely, WFH!!!
Now the Tories will say “4% rise if you will supervise PAs, 0% if you refuse…”
You will miss GPs and the NHS when it’s gone...
NHS has been waylaid to be like Kaiser Permanente
https://twitter.com/i/status/1616905011333586944
Select-right click-go to...
Please watch this terrifying video...
The NHS provides for everyone! Kaiser
and ACOs, ICBs only for
those selected...Systems like Kaiser Permenente and Valencia
They are given a budget, they decide how to spend this.
The SoS has no duty to provide a comprehensive health service.
They provide less care, to earn more profits
Inherently, need a provider and a purchaser
Kaiser were given NHS Kaiser beacon sites
United Health, Evercare made repeated attempts
McKinsey wrote the 2012 Lansley Monster Health Act
This provided harmony with US companies in a US UK trade deal
Centene, Optum were embedded in the NHS
Mental health is swamped with private profiteer firms
Many MPs, both Tory and Labour, are being groomed with
money!
These private, profiteer USA style health firms expect return favours!!!
Wes Streeting £193,225!!!
Keir Starmer £157,500
Stella Creasey £5,000
Yvette Cooper £231,817
Rachel Reeves £14,840
Angela Rayner £50,000
David Lammy £1,640
Many suspect Wes Streeting of being more Tory than Tory: he promises
-more privatisation (which-costs 30% more)
-has not the capacity,
-uses NHS teams,
-destabilises the NHS systems & specialities
-takes money from NHS taxpayers…
-Will not end purchaser/provider (takes 15%)
He
-Will not pay off PFI (eleven times the original cost…)
-Will not carry out DDRB reform, pay full pay restoration
-Will not end AAs and PAs to replace doctors…
Tufton Street think tanks, like Truss, Kate Andrews, Thiel (Palantir) like Trump, want to end the NHS
Totally build at least ONE state of the art, big new Hospital for Queen Elizabeth, Kings Lynn- (they have no land-instructed to sell it off years ago)
Having made Councils go bankrupt, now urge them to sell of the Town Hall, Libraries, Parks, Fresh air-privatise everything…
Same with the NHS-underfund it, sell off everything to private profiteers
Most citizen will pay tax for a good NHS and SC...
Important!!! Julia at EveryDoctor states that many NHS supporting MPs, both Tory, and expecially Labour have been told to shut up about improving the NHS
NHS Dentistry
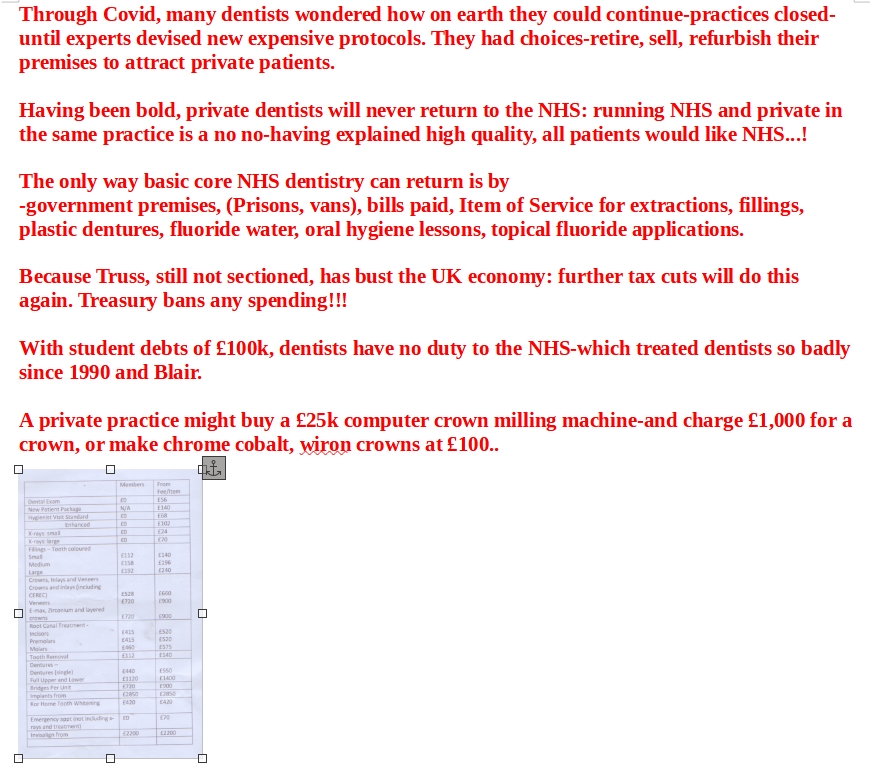
NHS Dentistry
I loved my profession-especially when I was single after divorce. I especially empathised with poorer patients-especially when dental NHS charges went up repeatedly (£3.50/£12 initially, £290 at present)
We bought a practice from a suicide dentist. We divorced.
In the beginning, after 1948, the Treasury panicked at the high initial cost of NHS dentistry-ignoring the cost would reduce after the initial years-and cut the fees.
Every decade, government have criticised high grossing dentists- even though, after expenses, net income was often below TargetAverageNetIncome.
Every year, government instructed DDRB to limit pay awards, whatever the justification, reasons for a better catch-up
Government ended the retrospective yearly correction of AVERAGED expenses, NOT INDIVIDUALISED expenses.
Hard working, long hours, dentists who provided chromes, crowns, bridges, veneers at no profit income, were criticised for high gross, their net income was unknown-and probably low
We sent accounts to Health Sec Virginia Bottomley; Peter Bottomley, MP, husband, said “these do not show not particularly high income…”
Fees were lowered- many did crowns, chromes, bridges only privately (selective withdrawal)
BDA reps who suggested going private had threats of homes seized by sequestration. Audfience members were primed to suggest this...
Dentists converted to private slowly- until forced closure during Covid prompted rejecting low NHS fees, upgrading to attract private patients, ceased accepting NHS…
The taxman vigorously attacked dentists: I had a £20k fine because my
accountant had increased car claims to 80% (unknown to me!!) I had to work harder
and intensively for years to recoup this (They went after my brother after…!)
After divorcing my partner, I had
£5k to spend on a new practice roof
£6k on a new Xray tubehead
£5k rendering-twice!
I had very high laboratory fees-no illegal selective withdrawal of lab items-but ostracised from the NHS for spending too much!
In many areas, NHS dentists formed a rota for emergency care. For one week,
each dentist opened his surgery for emergencies-a single contact number contacted
this dentist-and emergency care given.
I opened a surgery in my cow shed (conversion £5,000)-opened after hours,
and the NHS refused to pay me for approx 24 patients…
Dentists are taught to provide perfection-unlimited time for, say a crown preparation
Under the pre 1990 contract, the income after tax for a bonded crown was approx
£3…
Gold acrylic substandard crowns had a higher fee to encourage-most were soon
replaced!
Privately, for £110, (now £500+) a perfect crown could be provided.
The NHS banned white fillings under the NHS-amalgam dictated-this gave dentists a perfect entry into private fees for white fillings-an acid etched white filling takes approx 45 minutes
Politicians promised “the best” dentistry under the NHS, and Blair,
particularly, refused to take crowns from the NHS menu.
Nobody would question that the NHS should not provide implants, say, or cosmetic
veneers-but dentists always want to provide the best they can provide under
the NHS
The Dental Estimates Board (Rationing) -even suggested a 6”7”8 bridge
for a patient I had not even requested…
One dentist was banned by his principle from crowns, bridges-I did his bridges...
My partner principle requested a bridge-refused
I applied-accepted-a pure lottery…
Some restriction on menu items was needed-say, extractions, fillings, plastic dentures only-but no politician would promote such a two tier system!!!
Dental fitness-a truly elastic definition…
Edward Sampson said it was purposely such
to trap dentists who wanted to provide the very best they could wring from the
NHS-to trap those who only did very basic core extractions etc and left the
big holes untreated!
Making crowns, bridges, chromes illegal under the NHS would allow better fees for basics-including prevention…
Blair refused to do this!
Tory government strategies to dismantle the NHS
refuse full pay restoration, refuse to allow DDRB to be independent
outsourcing to profiteer cowboy firms
set up urgent care centres-Privately owned, privately run
can sell insurance, scans, diagnosticsa-just like Kaiser Permanente
employ PAs, nor real qualified GPs
flood our NHS with less qualified, less knowledgeable PAs and AAs-UNSUPERVISED!!!
Tory threats to our NHS:
-Same day hubs-staffed by any GPs? or by PAs, unsupervised?
miles away from your local GP surgery? do you register with them ? are they
on Item of Service? Privately owned, privately run? at whayt cost?
Purely to undernine and underpay GPs
PAs and AAs registered with GMC-so patients ate totally bamboozled... and believe they are doctors
Curb pay of frontline workers-esp pre-consultalts, ("Junior" Doctors) by knobbling the DDRB...
Article by Julia Patterson EveryDoctor
There’s a fierce debate going on at the moment about Physician Associates in the NHS, and so I thought it was time to examine what’s going on.
Physician associates aren’t a new concept; there have been a small group within the NHS since the early 2000s. However, they used to be referred to as “physician assistants”, and there weren’t very many at that time. The Conservative government, however, has decided to rapidly expand the numbers of physician associates (PAs), and anaesthetic associates (AAs), and they’re aiming to build a workforce of 10,000 PAs and 2000 AAs by 2036/2037, causing a huge amount of concern.
In order to explain why people are so worried, it’s important to understand the role they’re now expected to perform in the NHS, and the differences between a PA and a doctor.
Doctors go to medical school; this takes a minimum of four years (if you’re already a graduate and are being fast-tracked), but most people complete a medical degree in five. All medical degrees involve the same type of learning - lots of lectures and textbook learning, and also hundreds of hours of learning within clinical environments, where students are attached to different medical teams to learn about each speciality in turn. This learning continues once medical school ends and you qualify as a doctor. There is a structured training programme for foundation doctors - the first two years after you qualify as a doctor, when you rotate around many different specialities - and then you can apply competitively to a speciality training programme. All doctors - surgeons, GPs, hospital medics, the lot - have to undergo a rigorous specialist training programme involving postgraduate exams in order to train to become a fully qualified specialist in any givenarea of medicine.
The course, the training and the apprenticeships have been honed over decades. Medical training is gruelling and all-consuming, but it is consistent. If you move from one NHS hospital to another, or one area of the UK to another, you could walk into a hospital as a doctor, declare your level of training, and the team around you would have a pretty accurate idea of your level of expertise, and your need for supervision. This, incidentally, was really important during the pandemic. Teams were rapidly assembled and moved from one ward to another, and this ability to identify the level of experience of every member of the team was really important. In full PPE, it was difficult for staff members to see each others’ faces, and so many teams wrote their role – essentially their rank - on their faceguards with a pen in big letters (CONSULTANT, SHO, REGISTRAR) to enable a swift flow of decisions up and down the chain of command.
This hierarchy of decision-making is absolutely crucial in understanding the
debate around physician associates. Medicine has a strict hierarchy of supervision,
learning and decision-making, and that makes patients safe.
Physician associates are not doctors.
They do not go to medical school. They aregraduates who have a degree (“in a health, biomedical science or life-sciences subject”) and they then complete 2 years of postgraduate study to become a PA. They are trained with the “medical model” which means that they are taught to perform some of the tasks that doctors do; for example talking to a patient about their symptoms (which is called “taking a history”, or “clerking”), or examining a patient. They do not, however, have the grounding of medical knowledge that doctors have, and so it is often difficult for doctors to understand their professional limits. They might understand what an allergic rash looks like, for example, but do they understand the physiological mechanism taking place? They might understand when a blood test shows poor kidney function, but do they understand the anatomy of the kidneys? How much do they know about anaemia? The clotting cascade? Thyroid function? This is why, for so many of the doctors I’ve spoken to, they aren’t sure at what level to pitch their discussions with their PA colleagues. They don’t want to patronise their new PA colleagues, but they don’t want to assume a level of understanding either. All of this is highly stressful in busy clinical environments because, atthe moment, NHS doctors don’t have much time to stop and discuss the basis of disease. They’re rushed off their feet.
Because PAs are not doctors, they are also not allowed to prescribe medications, and so doctors are meant to supervise them. But this is causing problems too. After all, if things are extremely busy, doctors often don’t have time to supervise PAs all the time, and are now being put in compromising positions. Should they sign the prescription that a PA says is necessary for a patient? Can they trust the physical examination that has been performed? How accurate was the information that came from the PA’s clerking of the patients they have seen, and are they willing to put their signature to the decisions made off the back of this work?
From what I have heard, the situation varies wildly across the UK at the moment. There are NHS departments where PAs are receiving excellent supervision, and where they are a valued addition to a busy and well-functioning team where everyone understands their role. There are other places, however, where, due to chronic understaffing, it is difficult to offer PAs the supervision required. On top of this, many members of the public are extremely confused about their role.
Many of the patients I hear from are confused or worried about physician associates,
and when the BMA ran a survey towards the end of last year, they found the same
thing.
As The Guardian reported at the time:
“Many people are deeply confused about the growing number
of physician associates in the NHS and wrongly assume they are doctors, research
suggests..
57% of people have never heard of physician associates, even though they are already widely used. Some 41% said it was not always clear if they were being treated by a doctor or someone else, and 29% were not sure if they had been treated by a physician associate.”
Many patients are concerned that a physician associate could miss something badly wrong with them, and these fears have been worsened by examples where mistakes have been made. The most high-profile example of this is the death of Emily Chesterton, who died in November 2022. She had attended her GP surgery in North London, believed she was seeing a GP, but was seen by a physician associate. She was misdiagnosed and died of a pulmonary embolism and cardiac arrest. She was only 30 years old. This tragic case caused a rise in questions about PAs, and their role within the NHS.
There has also been an on-going discussion about whether the GMC (the General Medical Council, which regulates UK doctors) should regulate PAs and AAs too. This has been rumbling on for many months, but it all came to head on Monday in the House of Lords.
As Pulse magazine reported:
“Last night, peers debated the Anaesthesia Associates and Physician Associates
Order 2024, which has already been rubberstamped by the House of Commons. Former
Green Party leader Baroness Natalie Bennett had proposed a ‘fatal amendment’
to stop the order’s progress through Parliament, based on concerns that
it represents a significant constitutional change without the necessary parliamentary
oversight….
…However, due to lack of support from other peers, Baroness Bennett was
forced to withdraw the motion at the end of the debate, meaning the order has
been approved.”
All of this is written in confusing parliamentary lingo, but essentially it has been decided that the GMC will regulate physician associates and anaesthetic associates. This has caused a lot of consternation from a lot of doctors, who feel that this further blurs the line between the medical profession, and other healthcare professionals who are not doctors.
Beyond the confusion from patients, and the confusion about the role of PAs and AAs, and the concern about patient safety which are so pertinent because of the state of perma-crisis in the NHS, there is also the issue of pay.
Junior doctors in the UK are not paid very much, given their long years of study and how hard they have to work, and staggering amounts of student debt many have amassed simply to get out of medical school (up to £100,000 when they finally enter the workforce). They work long on-call shifts, hold a lot of responsibility, and work nights and weekends. So it is unsurprising that some are fairly unimpressed,that many PAs are being paid more money to hold less responsibility.
There are lots of posts circulating on social media about this, but here’s one example, which was in a letter to the editor of the BMJ last September:
“According to the current agenda for change pay scales, a newly appointed
band 7 physician associate (PA) working in inner London will earn £48874
for a 37.5-hour working week, while a foundation year 1 doctor working an unbanded
40-hour work week in the same hospital would earn £34,560, both with London-weighting
respectively.(2,3) This means that a newly qualified doctor earns around 34%
less than a newly qualified physician associate, despite working more hours.”
34% is quite a big pay difference, all things considered.
It’s not just junior doctors who are affected. Many GPs are being indirectly affected too. The government is awarding pots of funding called “ARRS funding” which enables GP surgeries to hire staff, but those staff cannot be doctors. GPs are therefore losing their jobs and other, non-doctor staff, are being hired in their place, causing anger from doctors, worry for their patients, and desperation too - I’ve even seen a petition that someone started on the government website, calling for doctors to be able to apply for physician associate jobs (the petition was rejected).
But more than anything, the situation with the rapid expansion of PAs and AAs is causing confusion about the UK government’s motivations? Why are they not supporting the workforce of doctors? Why are they not doing everything they can to retain doctors as well as hiring new, non-doctor staff? After all, all healthcare professionals have a role. In departments that are well-staffed and well-run, PAs and AAs would be a really valuable resource to any medical team. If we want to understand any of this, we need to stand back from the situation and think about it differently.
UK politicians are corporatising and privatising our public healthcare system. In the short term, they are creating conditions that de-skill our NHS workforce. They are doing this by failing to train enough doctors, failing to retain the doctors we do have, squeezing doctors’ pay and eroding their working conditions to encourage a mass medical exodus from the NHS. They are then intentionally recruiting lower-skilled staff en-masse (including PAs and AAs) and, initially, paying them better. It is unlikely this higher pay will last for the long-term because, ultimately, they are seeking to reduce the overall NHS staff wage bill.
Politicians are doing all of this to quietly rebuild the NHS from within; they are successfully creating a second-rate public healthcare system where patients have increasingly restricted access to skilled, senior medical decision-makers. They’re turning the role of a senior doctor from that of an expert delivering patient care, into a supervisor of lower skilled workers. In time this will reduce the staff wage bill significantly, debase the public healthcare system further, and allow further proliferation of private healthcare in the UK to fill the growing gaps in care this model creates.
This is neither fault of doctors or PAs; if we want to oppose the destruction of our NHS, we can’t get caught up in minutiae. Instead, we need to look at the big picture, and oppose NHS corporatisation and privatisation very strongly. We can push back against this and reverse the situation, but we must do so together.
Many of our community cannot afford a full subscription, but have asked to make
one-off donations when they can to show support- I appreciate this so much,
and anything you can give to help support my writing is massively appreciated.
If you’ve found this piece interesting, could you possibly consider sharing it?
© 2024 Dr Julia Grace Patterson
Hunt v Hawking
Why did health secretary Jeremy Hunt choose to have a public spat with Professor Stephen Hawking about statistical analysis and the future of the NHS? Accusing Hawking of spreading ‘pernicious falsehoods’ was a high-risk strategy, but Hunt has an ego, is proud of his record as health secretary and took the bait. Hawking suggested the NHS is heading towards a US-style insurance system, run by private companies, citing the increasing involvement of the private sector in the NHS as evidence for this. Hunt argued the government has no plans to introduce an insurance system and the private sector currently takes only 7.7% of the NHS budget. But as former Tory prime minister John Major during the Brexit debate; ‘Michael Gove wanted to privatise the NHS, Boris Johnson wished to charge people for health services and Ian Duncan Smith advocated moving to a social insurance system. The NHS is about as safe with them as a pet hamster would be with a hungry python.’
In 2005, Hunt co-authored a policy pamphlet with Gove, Douglas Carswell and others which proposed a universal insurance system for the NHS and stated; ‘Our ambition should be to break down the barriers between private and public provision, in effect denationalising the provision of health care in Britain.’ Hunt’s current position is that the NHS will remain ‘a single-payer system’, funded from general taxation, and by his definition would remain a public service even if all its services were privately provided. However, private provision transfers significant power and funds to profit-seeking shareholders and to many (including MD), that constitutes privatisation of the NHS.
Simon Stevens, the current NHS England chief is credited with accelerating
competition and private outsourcing under Tony Blair, later boosted by Andrew
Lansley’s health act, but the NHS is now having to live with the disastrous
consequences. A report by the Centre for Health and Public Interest has found
that in the last 6 years, companies that run PFI contracts for the NHS have
made pre-tax profits of £831 million that could have been spent on patient
care. In the next 5 years, £973 million of NHS funds will go to PFI companies.
And up to £4.5 billion been squandered on setting up, administering and
regulating a rolling program of competitive tendering in the NHS since 2012.
Hunt and Stevens stand no chance of making their planned £22 billion of
austerity savings by 2021 by fragmented competition.
Instead, the English NHS is trying to move to ‘place based planning’
where local services merge, rather than compete, in the form of 44 Sustainability
and Transformation Partnerships (Eyes passim). (Slash, trash and burn)
Each STP is expected to make its share of eye-watering savings, and some will
try to become Accountable Care Organizations.
As Hawking pointed out in The Guardian: ‘An ACO is a variant of a type
of US system called a health maintenance organisation in which all services
are provided in a network of hospitals and clinics all run by the HMO company.
It is reasonable to expect the powerful US HMO companies such as Kaiser Permanente
and United Health will be bidding for the huge contracts to run these ACOs.’
Hunt trumpeted Kaiser as a model for future NHS care at the Commons health select
committee in May 2016. The NHS could run its ACOs but Lansley's Health Act may
force it to put them out to international tender to Kaiser etc.
Other cunning plans to balance the NHS books include selling off its ‘redundant’
land and building assets to property developers on the cheap (see the Naylor
Review), encouraging the NHS to take on more private work and further discouraging
GPs from referring patients to hospital.
Referral management centres started under Labour but are escalating such that
all referrals will be triaged weekly by clinical peer review. A third of these
centres are currently run by private companies, the rest by the NHS at a total
cost of £57 million since April l 2013. Some patients may not need referral,
but others who need hospital treatment may be refused or delayed.
Hawking also criticised Hunt’s cherry picking of weekend mortality statistics
based on a single paper in the BMJ. Hunt’s defence was ‘that to
decide that one piece of research is the most credible is not cherry picking,
it is doing what you have to do when researchers disagree.’ Bollocks.
What you do is a systematic review of all the existing studies, not choose the
one you like the results of. Orthopaedic registrar Ben Dean discovered the updated
study originated from a request by Simon Stevens in a ‘7 day services
meeting’ involving senior NHS England members and Deloitte. So perhaps
not quite as independent as Hunt claims.
Before the paper had been properly peer reviewed and published, NHS England
was using it to justify changes to junior doctors’ contracts, and this
bad science subterfuge was one reason the conflict turned so sour. People may
die at weekends because of chance, because they are sicker than those admitted
during the week, or for lack of care. The deaths could be avoidable or non-avoidable.
If research shows more services are needed, it will probably need extra staff,
rather than shifting around the existing staff who can barely cover weekday
shifts.
The NHS could well be safer at the weekend but Hunt’s alienation of a
generation of junior doctors is unlikely to help.
If the NHS can really make £22 billion more savings without harming staff
and patients, Hunt and Stevens will deserve their place in history. MD’s
money is on the NHS struggling along in heavy debt, cutting services, increasing
waits and mopping up the crisis in social care that Theresa May is now too frightened
to address. Merging health and social care into a single ‘care’
system makes sense but is fiendishly hard to do if one is tax-funded, the other
is means-tested and the division is grossly unfair. For many, Nye Bevan’s
promise of state funded ‘cradle to grave care’ has long since vanished.
Many ophthalmic surgeons say they are able and willing to do more cataract ops-
but NHS will not pay for them
Many surgeons could clear waits, but cannot get operating time
More op theatres, and teams to work them are required
With more staff, more surgeons, after Full Pay Restoration, better use could
be made- even early morning or evening working
Frontline staff denied full pay restoration
Real Doctors, and the BMA are treated as the enemy by NHSEngland will not strive
harder, but work carefully, slowly, diligently, to rule.
Yesterday, NHS England laid out its changes for the 2024/25 contract. It is an imposition – like last year, it hasn’t been agreed with the BMA GP Committee.
The BMA will ballot GPs on whether to take further action, with industrial action later in the year a distinct possibility. But with no more negotiations on the horizon, this will be enforced from April 2024.
We take a look at what it means for practices.
FINANCIAL ASPECTS
The total increase in funding for general practice in England will be 2.23%
next year – an increase in investment of £259m taking overall contract
investment to £1,186m. However, it is highly unlikely that the global
sum will increase by this much. NHS England gave a breakdown of how it calculated
the £259m funding increase:
•2% pay increase for all GPs and practice staff – which it said
could increase once the DDRB has given its recommendations;
•2% uplift to the ARRS;
•1.68% inflation – which it claims is in line with the Government’s
November 2023 GDP deflator;
•0.38% ONS population growth.
This is all pretty bad news for GPs and practices. The £259m extra incorporates the population growth, which means that much of this funding will be covering the extra patients, and won’t increase payments per patient.
As well as this, the way the staff portion of the funding is calculated has been criticised by some GPs as being unrealistic – so if the DDRB does recommend increased pay for GPs and staff, the funding boost may not cover them, therefore eating into practice funding.
The upshot of all of this is that the increase in the global sum is – at best – going to be around 1.68% that is ‘in line with the Government’s November 2023 GDP deflator’.
But it is on this final point where the real scandal lies. Because anyone who has turned on the news, or had to pay a bill of any kind will know that there is a cost-of-living crisis due to inflation way beyond 1.38%. And even if it is argued that inflation is slowing, general practice missed out on inflationary increases in the past couple of years due to the five-year funding agreement from 2019.
As a further kick in the teeth, NHS England have said that any unspent ARRS money will be clawed back – with no commitment to keep it in general practice.
This obviously has gone down badly with GPs, the GPC and accountants. GPC England chair Dr Katie Bramall-Stainer said the ‘GP business model is now non-viable’, adding that this is ‘an intentional, predetermined, strategic, non-evidence based, ideological dismantling of NHS general practice’.
Andrew Pow, board member of the Association of Independent Specialist Medical Accountants, said ‘This is a disappointing announcement and the third year running when uplifts in the value of the GP contract have been significantly below inflation. While the contract is based on an assumption of 2% pay growth for staff, practices face significantly higher wage growth from April as a result of the near 10% increase in the minimum wage. This will also filter through to other pay bands.
‘The contract uplift allows for inflation at 1.68%, yet inflation is running at 4% in the economy. While energy costs may be on a downward trajectory and loan interest costs have hopefully flatlined, these costs remain far higher than they were a couple of years ago and were not funded in contract uplifts in the previous two years.’
QOF
Andy Pow says that there is good news for practices. Aspiration payments for QOF will increase from 70% to 80%, which will help with cashflow as more money will be paid through the year. Meanwhile, 42% of the QOF indicators will be suspended, with practices being paid for these based on previous years’ performance (though it is unclear which years).
The ‘protected’ indicators include:
•Mental health MH021: Providing physical checks to mental health patients,
such as smoking status, alcohol consumption and BMI (6 points);
•Depression DEP004: Reviewing patients with a new diagnosis of depression
(10 points)
•Asthma AST008: Recording smoking status of patients with asthma (6 points)
•COPD COPD014: Referring patients with COPD to a pulmonary rehabilitation
programme (2 points)
•Smoking SMOK005: Offer of support to smokers with respiratory or certain
mental health conditions (25 points)
•Cancer CAN004: Cancer patient who have had a Cancer Care Review in the
previous 12 months (6 points)
•Cancer CAN005: Cancer patients who have had the opportunity for a discussion
and informed of the support available from primary care, within three months
of diagnosis (2 points).
The majority of the protected points come from the disease registers, however – making up 81 points.
But for GPs in reality, this might be a bit underwhelming. The register indicators involve no clinical workload and only minimal administrative workload. Dr Gavin Jamie, a GP in Swindon who runs the QOF Database website, says: ‘The income protection for disease registers is meaningless.’
He points out that the only income protected indicators that will help workload ones are those for cancer.
That said, there is also income protection for the QI indicators, which involve the wellbeing of staff, optimising capacity and reducing avoidable appointments – these are worth 74 points. ‘These do genuinely take up a lot of admin time,’ says Dr Jamie.
The significant changes to the QOF are more likely to come as a result of the QOF consultation, which remains open until 7 March. Dr Jamie adds: ‘I am not sure why there is this “income protection” thing rather than just amending QOF. I suppose that they are keeping their options open for next year. This feels like a holding position!’
ARRS
The major change to the additional roles reimbursement scheme involves the inclusion of ‘enhanced nurses’. If this sounds confusing, that’s because it is.
Currently, advanced nurse practitioners are part of the ARRS. ‘Enhanced nurses’ is not a particularly well known term in general practice. As our sister title Nursing in Practice has reported, it is not currently a job role recorded by practices or PCNs for workforce data collection and there are no further details from NHS England about the new ARRS role at present. A core capabilities framework states that they are a level above registered nurses and below advanced and consultant level practice nurses.
It is likely that these are therefore going to be experienced practice nurses with a specialism in long-term conditions – but this remains speculation.
The other main change – other than the removal of unspent ARRS money – is the removal on caps on numbers of ‘direct patient care roles’ that ARRS money can be used for. These include ANPs, pharmacist, physiotherapist, paramedic, occupational therapist, dietitian or podiatrist.
Although, of course, the bigger problem is that the funding hasn’t increased beyond the not-even-inflationary rise. And an even bigger problem is that, despite the GPC’s (and Pulse’s) call for GPs to be included in the ARRS, they have not done this.
DATA AND CONTINUITY
Despite the contract letter lauding the cutting of red tape, NHS England can’t help itself, with more data collection requirements.
Practices will be required to provide data on eight metrics through a national
data extraction, for use by PCN clinical directors, ICBs and NHS England: call
volumes; calls abandoned; call times to answer; missed call volumes; wait time
before call abandoned; call backs requested; call backs made; average call length
time. This shouldn’t lead to greater workload, but this continues NHS
England’s focus on access and could lead to practices facing more awkward
questions.
Alongside this, there are new requirements around workforce and vaccinations data, while practices will be expected to produce a digital copy of their practice boundaries.
At the NHS Confederation conference yesterday before the contract was announced, NHS England primary care director Dr Amanda Doyle said that continuity of care will form part of the contract in future years. Later that day, it transpired she meant 2024/25. The letter says: ‘GP contract regulations will be amended to explicitly require continuity of care to be considered when determining the appropriate response when a patient contacts their practice.’
We will have to wait for the upcoming contract documents to see how they will measure and enforce this.
PCN DES
One of the ‘carrots’ given by NHS England has been simplifying the PCN DES by merging eight of the service specifications – medicines optimisation; enhanced health in care homes; early cancer diagnosis; social prescribing service; CVD prevention and diagnosis; tacking neighbourhood inequalities; anticipatory care; and personalised care – into one ‘simple overarching specification with a greater outcomes-focus’. The only separate service specification will be enhanced access.
It is not clear why this has been done, or what the agenda is behind this. The ‘greater outcomes-focus’ looms large. Until we receive the NHS England guidance, we will be none the wiser.
There have also been major changes to the Investment and Impact Fund (IIF) indicators (ie, the PCN equivalent of the QOF). They have been reduced from five to two – with those relating to flu and access being ditched, and those relating to learning disabilities and cancer remaining.
The funding from these retired indicators has been put into the Capacity and Access Payment, which requires PCNs to provide digital telephony, simpler online requests and faster care navigation.
There are changes to the clinical director role: funding will be rolled into core PCN funding, and there responsibilities are defined as ‘co-ordination of service delivery, allocation of resources, supporting transformation towards Modern General Practice and supporting the PCN role in Integrated Neighbourhood Teams’.
PERFORMANCE LIST CHANGES
The performance list flexibilities that were brought in during Covid. The letter says: ‘Supporting guidance will also be issued to clarify that non-GP doctors should not see undifferentiated patients, and that they continue to be required to operate within their sphere of competence.’
It adds that these changes will ‘permit GP practices and PCNs to employ doctors who are already employed, for example, by an NHS trust, NHS foundation trust or health board without the requirement for the doctor to also be registered on the medical practitioners list’.
This seems to open up the path for staff and associate specialist doctors to be employedby practices and PCNs (although they are not – as yet – part of the ARRS).
Yet the requirement that they should not see undifferentiated patients seems to prevent them from working in traditional general practice. And GPs might be forgiven for questioning why SAS doctors are not allowed to see undifferentiated patients, yet physician associates are…
WHAT IS NEXT
The BMA will put the contract to the profession next week. As it has been imposed, they will recommend that GPs vote against it (and it will be a huge surprise if ‘Yes to the contract’ polls 1% or above).
This won’t be news to NHS England, and with such a poor offer – especially in terms of funding – they are unlikely to negotiate to anything near what would be acceptable to the GPC negotiating team. GPC chair Dr Bramall-Stainer has said she expects the process to lead up to a general election in autumn, and the GPC leadership is not afraid to call for industrial action.
We have a long summer ahead.
Manifestos are works of fiction
Hopes, aims, lies to bribe thee electorate
Blair reversed pledge to reverse purchaser provider
Cameron did it with Lansley
Boris with 2021 Health bill although planned with Steven’s years earlier
This obviously has gone down badly with GPs, the GPC and accountants. GPC England chair Dr Katie Bramall-Stainer said the ‘GP business model is now non-viable’, adding that this is ‘an intentional, predetermined, strategic, non-evidence based, ideological dismantling of NHS general practice’.
Andrew Pow, board member of the Association of Independent Specialist Medical Accountants, said ‘This is a disappointing announcement and the third year running when uplifts in the value of the GP contract have been significantly below inflation. While the contract is based on an assumption of 2% pay growth for staff, practices face significantly higher wage growth from April as a result of the near 10% increase in the minimum wage. This will also filter through to other pay bands.
‘The contract uplift allows for inflation at 1.68%, yet inflation is
running at 4% in the economy. While energy costs may be on a downward trajectory
and loan interest costs have hopefully flatlined, these costs remain far higher
than they were a couple of years ago and were not funded in contract uplifts
in the previous two years.’
Dear Keir Starmer
The NHS is being dismantled through the Tories obsession with private US style
health insurance, privatisation and outsourcing to profiteer companies.
By cutting waste from
Not taxing Google, Amazon, oil highly and correctly
By waste of doctors, nurses, midwives, anaethetists leaving in drovesGPs being
driven out by PAs, unable to recruit new GPs through ARRS funding limited to
PAs
Allowing tax havens
Not recovering unpaid tax
Not recovering fraud
Governments pretend there is no money
Can you pledge to be a proper centre socialist party
And stop the intentional dismantling of the NHS, just as NHS dentistry has been
withered on the vine.
Full pay restoration is urgent
Stop PAs, AAs
Invest in at least one new, completely rebuilt hospital- Queen Elizabeth in
Kings Lynn is held up by Acrow props
Maternity is unsafe
GPS have been bludgeoned into quitting and closing practices.
Campaigners have urged to Tories to stop destruction (purchaser provider, Any
(Un)Qualified Provider, Lansleys Monster2012 Act, 2021 Health and Social Care
Act-All allowed to pass by ignorant politicians
Now PAs, AAs, registered by General Medical Council (£800k- £2 million
bung)
All designed to form a Soweto third world NHS… Social Care now non existent,
We know manifestos are just hopeful fiction, can be reversed after election
But the
UK needs a functioning NHS staffed by UK trained workforce- not poaching foreign
workers with false promises- they will leave once they see the state politicians
have left the country.
Let the NHS be the one Labour achievement that is improved, not destroyed by your government if elected