The NHS and Social Care is under threat on so many fronts-
The extreme right wing-Kate Andrews, Liz Truss, Hunt, Thiel, Trump
What is more worrying is that Liz Truss herself has embraced many of the right
wing policies and “solutions”. She is one of an 8-strong Parliamentary
Board of the 1828 Committee, whose ‘Neoliberal Manifesto’, published
jointly with the Adam Smith Institute in 2019, condemns the NHS record as “deplorable”
and calls for the UK to “emulate the social health insurance systems as
exist in countries such as Switzerland, Belgium, the Netherlands, Germany and
Israel, among others.”
The Manifesto is silent on the fact that (with the exception of the deeply flawed
Israeli system) all of its preferred models spend much more per head on health
than the UK.
All NHS Doctors, Surgeons and specialists, even dentists, advocate
for the best treatment
IVF for fertilisation
Cosmetic for best procedures
Orthopaedic for best procedures
I might want my legs lengtheneed, shortened-but not “necessary”
for health…
Rationing-by NICE for drugs
Prior approval for special treatments
Pharma
Companies like Vertex in Boston have newly developed very effective, but very
expensive drugs for cystic fibrosis, type 1 diabetes,
new drugs require expensive research, trials, safety, return on investment for
shareholders, and investment for the next invention
Pharma companies have many new drugs in the expensive pipeline from discovery
to production and purchase by governments
Research testing, trials and safety are extremely expensive.
Shareholders require a return on huge investments, and income from one drug
funds development of the next.
Vertex in the US have very effective new drugs for cystic fibrosis and type
1 diabetes- both leading to better treatments
The UK government has not yet purchased these- but with negotiation, the initial
high cost can be modified.
A new ring fenced tax-purely four the NHS and Social Care, starting at age forty,
can enable better treatments- but Nice has to see that these are cost effective…
NHS Dentistry
NHS dentists all wanted to pay their staff well, pay good quality lab technicians promptly each month, invest in good equipment, fibre optic hand pieces, intra oral cameras, good ultrasonic and air scalers, curing lights, materials and take time over new techniques…
The Dental Rates Study Group awarded lower and lower fees, dictated by averaged
expenses, not individualised.
Government ceased the agreed annual updating of expenses arrears.
The DDRBody was told the % award, despite evidence for higher awards
They were used to slow other groups pay.
The Gulf war return of oxygen cylinders caused most to cease extractions under
GA, most private child subscription schemes send children to hospital to avoid
denting their reputation.
Low fees for children’s dentistry-using capitation essentially stopped
child fillings.
Same day hubs
These privately-owned and run centres, manned by PAs(?), GPs (maybe), take resources from GP partnerships, reduce practice viability
GP surgeries have been starved of funds-under ARMs contract, can affortd PAs,
not real GPs
They may sell private health insurance, refer for private tests, diagnostics,
scans… as in the Kaiser Permanente system...
After the arm twisting, threats and promises that led to Lansley Monster Act 2010 being passed, I am sure many in the BMA, Royal Colleges like Clare Gerada have been urged to support Physician Associates-lower trained non-doctors, to substitute for real doctors in the NHS and GP surgeries...
The extreme right wing (Regan, Thatcher, McKinsey, Truss, Letwin, Redwood-”Lets
privatise the World”)
want a “smaller state”-ie we pay more for services and pay less
tax-esp the richer
Many are happy to pay more tax (inc the Davos millionaires) for better public services
In the UK, we pay less for the NHS and Social Care, and pensions-than most of Europe
Our NHS has fewer Doctors, Nurses, Beds, Maternity frontline…
fewest scanners, diagnostics IN THE NHS-many PRIVATE-outside the NHS
and the UK Tories waste humongous amounts on
Mone PPI
T & T Di do,
undertax Google, Amazon
An overworked, underpaid GP should be able to fill a web form to refer a patient-not
wait on a telephone for several calls-without being bounced back by a pimply
youth to save money... for "advice"
The Kaiser Permanente Accountable Care Organisation model favoured in the UK
tries to keep patients out of (expensive) hospital care, by unloading droves
of patients into non-existant “community" care-ie GPs
but GP funding share is now at lowest 8.4%, hospital care funding at highest
In 2019 6000 more GPs “promised”
now, fewer full time GPs, workload increased by 20%
Osbourne cut Training places (four years + five years at medical school: eleven, £100,000 debt for GPs)
46% of GPs come from abroad- need housing, UK citizenship or they leave
England needs 16,700 more GPs to match OECD average per 10,000
Hospitals offload much more onto GPs
After a year waiting, consultants bump off the waiting list-to be “managed
by GP”
see below...
Tories are delaying negotiations for Full Pay Restoration in the hope that winter passes, and the electorate forget the Junior doctors, and AAs and PAs take over the asylum...
The Lowdown
From The Lowdown (Excellent!)
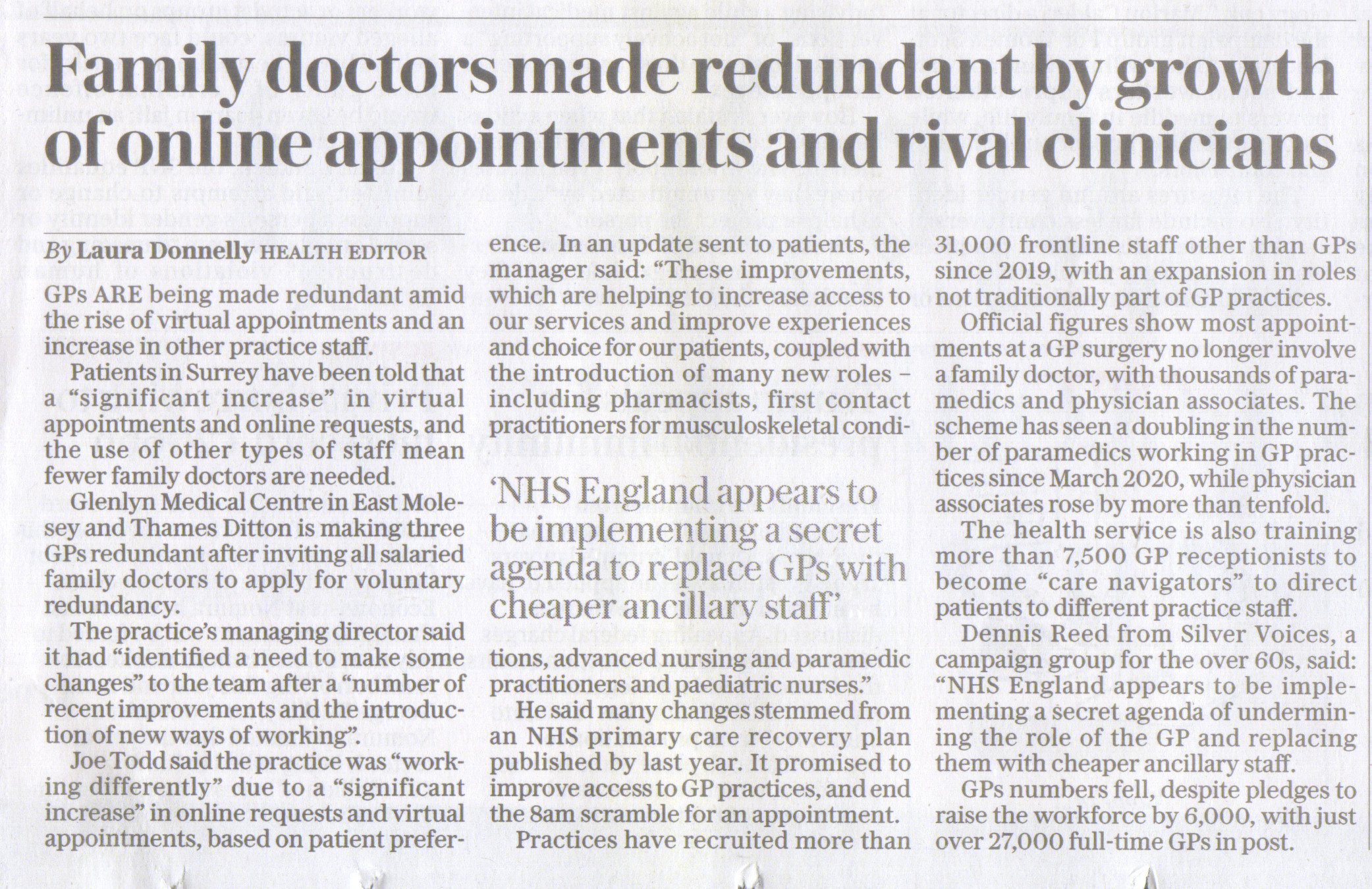
The increasing use of physician associates (PAs) within the NHS has hit the headlines in recent months, with numerous social media discussions, many of which has been acrimonious, and negative headlines in the mainstream media about their work.
Such is the concern over their use, and the related profession of anaesthetic associate (AA), that the BMA and the Royal College of Anaesthetists, have called for a pause in recruitment and the GMC has called on NHS England to confirm there is no plan to replace doctors with PAs.
PAs have worked within the NHS for 20 years, as have AAs and related positions that all come under the grouping medical associate professionals or MAPs. So what has happened to trigger the current debate and outcry over their use?
The media spotlight comes at a time of increasing recruitment of medical associate professionals (MAPs) within the NHS, primarily PAs and AAs, following a pledge within the long-term workforce plan published in June 2023. PA numbers are planned to increase to 10,000 by 2036-37 ( from around 3,000 at present) and AA numbers to 2,000 (from around 120 according to recent figures). This increase in number is a key component of the workforce plan. And PAs, in particular, are becoming more visible to the general public as their numbers increase.
Plus, the mainstream media picked up on two tragic cases of deaths due to mistakes made by PAs in GP surgeries.
Emily Chesterton died in November 2022 after a PA failed to diagnose and treat her deep vein thrombosis and pulmonary embolus at two consultations and did not seek advice from a GP, and Colleen Howe, died in 2023 from aggressive breast cancer after delays caused by a misdiagnosis from a PA at her GP surgery.
These deaths highlighted the increasing use of PAs in GP surgeries and the lack of public understanding of the role. In both cases neither patient was aware that they were not seeing a professional that was not as well qualified as a GP.
Other social media discussions and media headlines have focused on PAs being used in positions that would previously have been the preserve of doctors. Recent headlines include the BBC revealing that Birmingham Children’s Hospital was using PAs in senior roles in the liver unit with a consultant on call. PAs have worked at Birmingham Children’s Hospital for 10 years but the BBC reported that it saw rotas which show them on tier two, normally a rota for senior doctors (registrars).
The discourse surrounding PAs on social media has been highly critical and acrimonious. The BMA has accused PAs of presenting themselves as GPs, doctors and consultants, and noting that there have been reports of medical students losing out to PAs for training. Plus there are reports of situations where PAs appear to be carrying out work that is outside of their remit.
Where do PAs fit into the NHS
Physician assistants, as they were originally known, were first introduced in the US in the 1960s to ease physician shortages. In the UK, PAs began work in 2003, and from 2013 they became known as associates rather than assistants.
PAs work as part of a multidisciplinary team with supervision from a named senior doctor (GMC registered consultant or GP), providing care to patients in primary, secondary and community care environments. AAs work under supervision in a similar way but only in the anesthesia setting.
The MAP grouping also includes Surgical Care Practitioners (SCPs) whose main responsibility is to support surgeons and other healthcare professionals before, during and after minor surgical procedures. Unlike PAs and AAs, SCP roles can only be taken up by individuals who are already registered healthcare professionals.
Training
Much of the media discussion has focused on the level of training that PAs/AAs receive before being allowed to work with patients.
To qualify as a PA in the UK, students had to have completed a bioscience-related first degree and then a postgraduate (level 7, i.e. a master’s level) degree in physician associate studies that takes two years. However, there are now undergraduate integrated Master of Physician Associate Studies programmes available that require A-levels or equivalent for entry and there is also a level 7 apprenticeship.
Registered healthcare professionals, such as a nurse, allied health professional or midwife can also apply to become a PA.
A PA can carry out a wide variety of work, including taking medical histories from patients, carrying out physical examinations, carrying out diagnostic and therapeutic procedures, and seeing patients with undifferentiated diagnoses.
However, they can not prescribe or request ionising radiation (eg chest X-ray or CT scan).
Regulation
In 2005 the UK Association of Physician Associates was established. In 2006 the Department of Health released a competency framework for PAs in conjunction with the Royal Colleges of Physicians and General Practitioners. A voluntary register was founded in 2011.
In 2015 the Faculty of Physician Associates (FPA) was established by the Royal College of Physicians to set standards and to oversee the PA-managed register. This register is voluntary.
Currently, PAs and AAs are not subject to any form of statutory regulation, but this is due to change. In July 2019, the Department of Health and Social Care (DHSC) asked the General Medical Council to regulate MAPs, including PAs and AAs.
In February 2023, the DHSC launched a consultation on PA regulation, which included extending prescribing responsibilities to PAs. This has closed now and regulation is expected for the PA and AA profession by the end of 2024.
What are the issues
The debate on the use of PAs and AAs in the NHS has highlighted a number
of issues including:
•the pay differential between PAs and junior doctors, with newly qualified
PAs earning around 35% more than junior doctors despite the difference in experience
and responsibility;
•a reduction in training situations for medical students;
•concerns over patient confusion as to whether they are seeing a PA or
doctor;
•and, the increasing use of PAs in GP surgeries in place of GPs.
In September 2023, the BMA published a position statement on PAs and AAs. In it the BMA noted:
“Patients should always know who is treating them and when this is – and is not – a medically qualified doctor….Patients and their families are often unaware they have not been seen or assessed by a doctor; such confusion is understandable – on social media there is a proliferation of physician associates (PAs) describing themselves as doctors, GPs, and medical consultants.”
On the pay differential, the BMA notes that it is:
“clearly wrong that a newly qualified doctor entering postgraduate training is paid over £11,000 less per year than a newly qualified PA, while the doctor’s role, remit and professional responsibility is far greater. We estimate that this is a 35% differential, which is manifestly unjust.”
To reduce patient confusion, the BMA wants a return to the title physician assistants. Anaesthesia associates (AAs) were similarly previously known as physician’s assistants (anaesthesia). Patient confusion will also not be helped, the BMA feels, by the planned move for the GMC to regulate PAs and AAs.
But the BMA’s objections to the current expansion of PAs and AAs goes far deeper that titles and regulator:
“Their use and planned expansion challenges what it means to be a doctor, reflects how the medical profession has been devalued, and demonstrates how the health system is seeking to undermine it in favour of colleagues with less training, skills and expertise.”
The BMA opposes the planned expansion of PA and AA roles, and the granting of prescribing rights following regulation, unless it can be demonstrated that the concerns have been addressed.
This month the BMA called for an immediate pause on all recruitment of Medical Associate Professionals (MAPs) in the UK including PAs and AAsacross general practice and PCNs.
Doctors from across the UK who make up the BMA’s UK Council passed a Motion calling for the moratorium on the grounds of patient safety. They want the pause to last until the government and NHS put guarantees in place to make sure that MAPs are properly regulated and supervised.
Previously, in late October, the BMA junior doctors committee and GP registrars committee published a statement on MAPs (medical associate professionals), noting that:
“in response to the manufactured workforce shortage of nearly 10,000 doctors, the rapid expansion of medical associate professionals (MAPs)…is detrimental to the provision of high-quality healthcare and represents a long-term risk to patient safety.”
The Royal College of Anaesthetists convened an extraordinary general meeting in mid-October at which over 90% voted to pause the rollout of AAs.
The GMC has written to NHS England, according to a report in HSJ, asking it to: “Directly tackle the perception that there is a plan for the health services to ‘replace’ doctors with PAs or AAs by convening and leading a system-wide discussion on an agreed vision for these roles.”
The national medical director at NHSE, Steve Powis, said in response to the GMC’s letter that there was no plan to replace doctors in the NHS.
Why have the GMC sold their soul, like Faust, to the devil, for £800,000-to legalise PAs and AAs???
The victims of the tainted blood scandal (we were told in 1968 of the risks!) should be paid by March 31st-no ifs, no buts...
The Treasury have for many years told the DDRB what maximum % they can award-to keep other public sector wages down-result: 26% pay loss...
Follow Medical twitter and @BSmytheee on Twitter to see the discussions, and Stephen Ross Sanford on Facebook...
Your General Practice frontline staff are providing a truly excellent service despite all the limits in funding, staffing, short staffing
Please do not take out your our frustrations on our workers!
The receptionist cannot magic appointments out of thin air!
Doctors work on their days off, for long hours trying to care for all patients
The ARP system does not pay for a practice to recruit more doctors-only paramedical staff.
There is a government limited shortage of medics, and training places for accreditation
Take time to say "you are doing a grand job despite the government"!
GPs will never strike: they will simply leave, one by one, and NHS GP practices close...
You will miss them when they're gone!
Fujitsu and the NHS, Post Office
from The Daily Star...
In 2002 Fujitsu won big contracts on New Labour’s NHS National Programme for IT (NHSPfIT). This was supposed to digitise NHS communications and records. NHSPfIT largely failed and Fujitsu were kicked off the contract in 2009, as the government claimed their systems were not ready and working on time.
Fujitsu responded by suing the government.
A clause in the contract said that, in the event of disagreement, Fujitsu could ask the London Court of International Arbitration (LCIA) to decide who was right. The LCIA is not an actual court, but rather a secretive, privately run, business-friendly arbitrator.
It was a big mistake for the government to give the LCIA the final word. Unlike real courts the LCIA does not report its decisions, but Fujitsu reportedly won its claim against the government: company accounts suggest they got all but £71m of their £700m claim .
It looks like an ugly picture: a firm behind a series of public-sector failures, which is implicated, morally at least, in a major injustice that saw innocent people go to jail — and which sued the government for hundreds of millions of pounds, taking money out of the NHS budget for an IT system that failed.
And yet the government is still handing Fujitsu contracts worth hundreds of millions covering tax, post-Brexit customs, defence and more.
Mostly this is because the government is still heavily focused on privatising services and does not have the capacity for running its own IT systems. The government finds it easier to sign single deals with large contractors and there are not many IT companies with big capacity like Fujitsu.
As with all privatisation, there is also an element of lobbying. Until 2019, Fujitsu UK’s chairman was Simon Blagden, a major Tory donor who gave party around £200,000 — Fujitsu say this was his personal money and not connected to the firm.
More directly, for many years Fujtitsu has paid both Tory and Labour parties to have a Fujitsu Lounge slap bang in the middle of their party conferences. When party conferences resume this year, I hope any MP sitting comfortably in the Fujitsu lounge gives a thought to the subpostmasters.
I asked Fujitsu about their responsibility for the subpostmasters persecution. They told me: “Fujitsu was not a party to the recent Court of Appeal proceedings relating to subpostmasters’ criminal convictions and so is not in a position to comment. We are continuing to co-operate with the ongoing Post Office Horizon IT inquiry.”
Palentir also greased their way into government-and boast that "once we are the main NHS software, they will have to like us"
Each practice should have their own computer data server-so when the UK system fails, appointments can still go ahead.
The failures to repudiate the Lansley Monster bill
-which REMOVED THE RESPONSIBILITY OF THE SOS HEALTH TO PROVIDE A COMPREHENSIVE HEALTH SERVICE
Please read NHS SOS to see the depths Tories will go to pass this privatisation bill...
The BMA failed at that time run by establishment Meldrum
The Lib Dems failed Shirley Williams, ignored the grassroots...
The Royal Colleges failed-threatened charitable status, "will be sidelined"
all pressured to agree...
The 2021 Health and Social Care bill
-which also REMOVED THE RESPONSIBILITY OF THE SOS HEALTH TO PROVIDE A COMPREHENSIVE HEALTH SERVICE
The UK has a rich knowledge base on healthcare, the best clinicians and campaigners
all suggesting to the Tories-whose Cabinet ministers have next to no interest,
knowledge nor understanding of the NHS and Social care improvements, elimination
of waste and best use of funds.
The Tories are bent on destruction of the NHS with private US style private
profiteer health insurance so they can siphon off taxpayers cash to their cronies,
with Labour chasing behind. The Tories have no mandate for dismantling the NHS.
Keir Starmer £157,000
Stella Creasey £5,000
Yvette Cooper £231,817
Rachel Reeves £14,840
Angela Rayner £50,000
David Lammy £1640
Wes Streeting £193,225
Lord Nash £237,000 to Tories (Care UK)
Stuart Rose (Practice Plus, Bridgepoint)
Steve Brine Remedium partners paid £20,000 (Sigma Pharmaceuticals)
Sigma won £100,000 contract LFTests
Jonathan Djangoly Pembroke VCT
Richard Fuller Investcorp Cambio Healthcare
The Byline Intelligence Team also found numerous links among the Conservative Party to other private healthcare interests.
Steve Brine, MP for Winchester, is a strategic advisor to Remedium Partners, a healthcare recruitment service. He is also paid £20,000 for up to eight hours of work a month as a strategic adviser to Sigma Pharmaceuticals.
Brine and Sigma took part in a video meeting in February with Nadhim Zahawi, the then Vaccines Minister. In April, Sigma won a £100,000 contract to deliver lateral flow tests to pharmacies. Bharat Shah, the founder of Sigma, told The Times that Brine was an advisor to the company and not a lobbyist. He said that Brine “was not involved with or had any knowledge of” the lateral flow test contract.
Meanwhile, Huntingdon’s MP Jonathan Djangoly has a second job as chairman of Pembroke VCT, which has invested in healthcare software companies.
His colleague Richard Fuller, who represents North East Bedfordshire, is an advisory director of Investcorp – a firm that has invested in Cambio Healthcare, which operates in the electronic health records market, offering software solutions for acute, primary, social and person-centred care.
North Herefordshire MP Bill Wiggin is a non-executive director at AllPay Limited, which recently confirmed a contract with the NHS Business Services Authority to facilitate payment card top-ups to the digitised ‘Healthy Start’ scheme.
Former Conservative Party leader Iain Duncan Smith is also paid £20,000 by Tunstall Healthcare; while former Health Secretary Jeremy Hunt has been paid £4,800 and £10,000 respectively for “speaking engagements” with Octopus Ventures – which backs “pioneers who are transforming the health industry” – and Penn Medicine London.
Other examples include Trade Minister Penny Mordaunt, who received £6,900 for speaking to the Boston Consulting Group – a firm that reportedly charged £10 million to assist the Government’s ‘Test and Trace’ programme.
Conservative MP Andrew Mitchell received £30,000 a year as a senior advisor
to UK Global Health Care from July 2017 to February 2020.
Prominent Brexiter John Redwood also had a £5,000 a year contract advising
EPIC Private Equity, which owns equity in the delivery service Pharmacy2U.
james-bethell-boris-johnson
Lord Bethell’s Summit with
Private Health Interests
Over NHS Reforms
Sam Bright and Sian Norris
Then there are donations from firms linked to private healthcare interests...
Hunt received a donation of £20,000 in June 2019 from Mustafa Mohammed,
the owner of Genix Healthcare, a private dental care provider.
Former Health and Social Care Secretary Matt Hancock received a £10,000 donation for his 2019 Conservative leadership campaign from Wol Kolade, head of Livingbridge, a private equity firm that owns Vanguard Healthcare. Kolade has donated more than £360,000 to the Conservative Party since the start of 2019.
Meanwhile, Dominic Raab’s 2019 General Election campaign received donations from Dominic Burke, whose Marsh & Mclennan subsidiaries provide healthcare insurance reports for private providers including AXA, Bupa, and Vitality Health.
The Government appears to be relying more and more on private healthcare providers through its ‘National Increasing Capacity Network‘. The initiative, which came into force in April 2021, has awarded a £2.5 billion contract across four years to numerous private providers, including those featured in the £1.69 billion contracts dedicated to increasing NHS capacity during the Coronavirus pandemic.
Companies listed on the National Increasing Capacity Network also have links
to Conservative donors.
Lord Michael Farmer, who has donated more than £6.5 million to the Conservatives
since 2010, is a shareholder in Centene which runs Operose Health – one
of 67 suppliers awarded a place on a separate Government framework contract
worth in total £10 billion in order to increase NHS capacity
Byline Times:
Tories raking in money from private health firms as NHS is on its knees
A number of high ranking and wealthy Conservative party members have links to
private health care companies which, in turn, are profiting from the current
NHS crisis
Penny Mordaunt took a £10,000 donation from care home firm Renaissance
Care UK
Tory MPs, lords and even Downing Street advisers have been shamelessly accepting
money from private healthcare firms as the NHS is on its knees.
Today we reveal connections between wealthy Conservatives and companies which
are profiting from the health service crisis.
The troubling links come as the Government dishes out contracts to the private
sector to tackle long NHS waiting lists.
And they emerge as private health providers cash in through growing numbers
of desperate NHS patients digging into savings for treatment.
Dr Megan Smith, an NHS anaesthetist in London and member of campaign group EveryDoctor,
said of our revelations: “This is sickening. It is the epitome of letting
the fox into the hen house.
“Private healthcare firms, in effect, paying for access to politicians
and obtaining benefits from cosying up to them undermines the integrity of our
NHS.
Dan Poulter is an NHS doctor paid £30k a year by a medical cannabis firm
Jonathan Djanogly is a chairman of a company that has invested in healthcare
software firms
“These links confirm this Government is a clear danger to the NHS and
public health.”
At least 28 Tory MPs and Lords have had ties to private health and medical groups, publicly accessible records reveal. There is no suggestion of wrongdoing.
They include: Suffolk MP Dan Poulter, an NHS doctor paid £30k a year
by medical cannabis firm Kanabo Group PLC
Wimbledon MP Stephen Hammond who earns £25,000 a year as a non-executive
director at Optibiotix Health that sells products to manage chronic lifestyle
diseases.
Huntingdon MP Jonathan Djanogly, the £30,000-a-year chairman of Pembroke
VCT, which has invested in healthcare software companies.
Steve Brine made £200 an hour giving 'strategic advice' to drug firm Sigma
Tom Tugendhat has shares in Accurx Ltd
Ex-health minister Steve Brine made £200 an hour giving “strategic
advice” to drug firm Sigma before resigning in 2021.
He earned £1,600 for eight hours a month as adviser to healthcare recruitment
service Remedium.
Portsmouth MP Penny Mordaunt, who made a bid for the Tory party leadership,
took a £10,000 donation from care home firm Renaissance Care UK.
She was also paid £6,900 for speaking to the Boston Consulting Group,
which made millions from Covid testing.
Security minister Tom Tugendhat has shares in Accurx Ltd – a software
firm “improving communication in healthcare”.
Richard Fuller was paid £20,000 a year as an adviser at Investcorp
Lord Greville Howard is a shareholder in two health firms
MP Richard Fuller, who represents North East Bedfordshire, was paid £20,000
a year as an adviser at Investcorp until last summer. The firm invested in Cambio
Healthcare in the electronic health records market. Mr Fuller had no hand in
that decision.
Chancellor Jeremy Hunt earned £12,000 for a speech to Healthcare Business
International, which provides services to “for-profit health care services”.
Unlike some colleagues, he donated the cash to charity.
Wokingham MP John Redwood has a £5,000-a-year deal advising EPIC Private
Equity, which invests in private prescriptions delivery firm Pharmacy2U.
Former Health Secretary Sajid Javid had share options in a California tech firm
behind health sector software. He sold his stake after Labour accused him of
a conflict of interest.
Lord Michael Farmer has shares in a US healthcare firm
Tory MP for Don Valley, Nick Fletcher, has an £800-a-month perks package
as a director of Analogue Electrics, which includes private health insurance.
Snouts in the trough are not confined to the Commons.
At least 16 Tory peers have interests in private healthcare and biomedical firms,
including:
Lord Michael Farmer, who has donated millions to the party since 2010. He has
shares in Centene, a US healthcare firm.
Its subsidiary Operose Health has taken over dozens of London medical practices.
Jeremy Hunt earned £12,000 for a speech to Healthcare Business International
He is also a shareholder in the US-based healthcare insurance company eHealth.
Baroness Blackwood of North Oxford is an equity partner for venture capital
firm Recode Health Ventures and chair of the advisory board of private blood
tester Thriva.
Lord Howard of Rising is a shareholder in medical diagnostics firms EKF, Renalytics
and kidney transplant tests company Verici Dx.
Lord Nash – who has donated more than £237,000 to the Tories since
2010 – has shares in private care homes provider Care UK, his register
of interests states.
Staff who work for a government bent on privatising the NHS have also had links
with health firms.
Boris Johnson with Dr Ashraf Chohan
Last February, Boris Johnson made ex-private health executive Samantha Jones
No 10’s Head of People.
She had been chief of Operose.
In November, Rishi Sunak gave Bill Morgan – a founder of lobbying firm
Evoke Incisive Health – a job as health policy adviser, where he is believed
to be helping drive through NHS “efficiencies”.
Evoke Incisive Health says it aims to solve “the most complex of challenges
in today’s healthcare market”.
John Redwood has a £5,000-a-year deal advising EPIC Private Equity which
invests in Pharmacy2U
A government spokesman said: “The MPs’ Code of Conduct sets out
the rules on the Registration and Declaration of Members’ Interests. The
Commissioner for Standards has given no indication these disclosures weren’t
made in full accordance with rules.”
A Conservative Party spokesman added: “This list pales compared to the
millions unions donate to Labour, resulting in MPs ordered to vote against laws
to keep the public safe in strikes.”
But a Labour source said: “The best advert for private healthcare is long
NHS waiting times. The Tories have delivered the longest in history. Private
healthcare has never had it so good.”
Under-fire Nadhim Zahawi racked up £1,000 limousine bill in one day at Cop26 summit
UK private medical insurance
Pre existing conditions are rarely covered: my wife cannot afford to join BUPA because she has a few pre-existing conditions
I joined BUPA 2021 at Dental school; now the monthly sub is £570- £6700 a year. BUPAs fees to surgeons have been pegged and capped. My hand surgeon collated BUPAs fees from 30 years back-present fees are lower…
My son in Boston, US, has med insurance from his very high-end employer-between them, for $25,000 a year, he, his wife, and child get full medical cover, maternity, ambulance, dental… BUPA say they cannot provide such cover.
BUPA seems to have disadvantages-very high costs, limited treatment, surgeons
fees capped and lowered
I has a top up requested after my brilliant hip surgeon replace my hip., plus
crutches, lav seat…!
Private teams take teams away from NHS hospitals, ophthalmic cataracts take
training from the NHS, close whole NHS departments
Notts dermatologists refuse to work outsourced-NHS team loses its pre-eminent
position…
Changing insurer has worries
will the new cover past treatments-or are they now pre existing?
Is the cover identical?
Their whole pre-authorisation procedure is clunky and unfit for purpose
we need one phone number for authorisations
no thirty minute wait
better hi fi phone equipment at their end: muted, indistinguishable, blurred,
cannot understand…
muti menu security and choices-terrible!!!
BUPAs website is very confusing-nowhere does it give a seperate number for
authorisations
seperate app-very clunky
BUPA touch dash
My consultant says What do you think to BUPA? He has chosen a different operator…!